We have no shortage in remarkable ideas – let us help execute yours
We are a dynamic team with combined experience of more than 20 years in all services we offer. Technology has opened doors for print, hence, we set no boundaries between print and digital.
We connect people, business and clients, in addition to promoting opportunities via our print/digital platforms. We are problem-solvers and offer impactful solutions with a holistic approach towards meeting and exceeding our client’s marketing/advertising needs.
Our services include
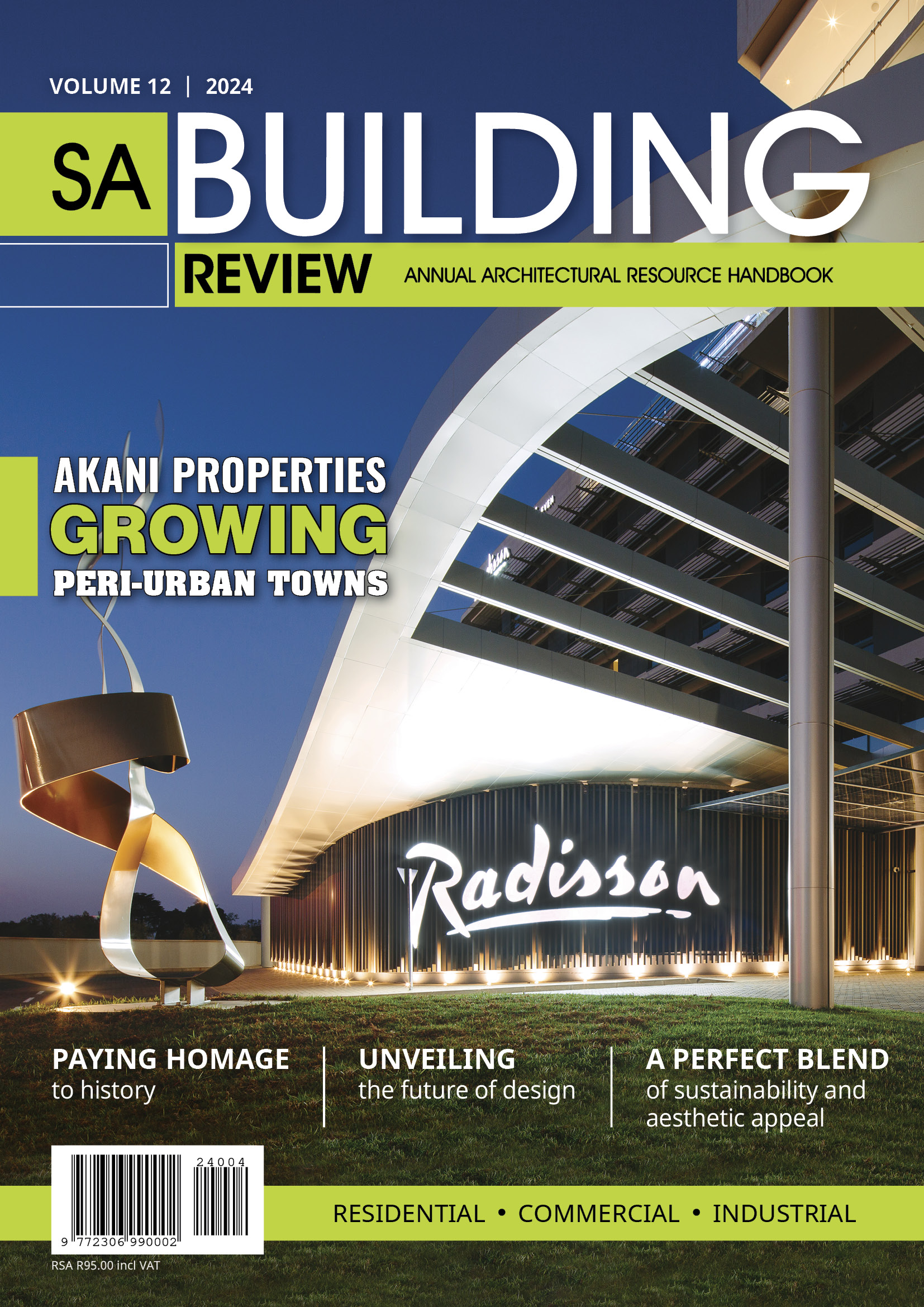
Publishing
Magazines, Magazine Supplements, Coffee Table Books, Annual Reports, Product Catalogues
Graphic Design
Letterheads, Logo’s, Business Cards, Email Signatures, Brochures, Pamphlets, Invitations, Advert Designs, Banners and much more…
Website Design
Custom website design packages available on request
Website Hosting
Payment options available when you host with us
Social Media Management
Content creation and management to boost engagement
Event Management
Our Publications
Magazines published
Total digital followers
Annual web visits

Year Established
Meet some of our clients…
What’s New at Media Xpose
Media Xpose crowned Magazine Publishing Company of the Year
Media Xpose, a South African based publishing house, were awarded top hounours at the Corporate LiveWire Innovation & Excellence Awards 2024 as Magazine Publishing Company of the Year. Nonimees from all over the world were critiqued on a number of factors...
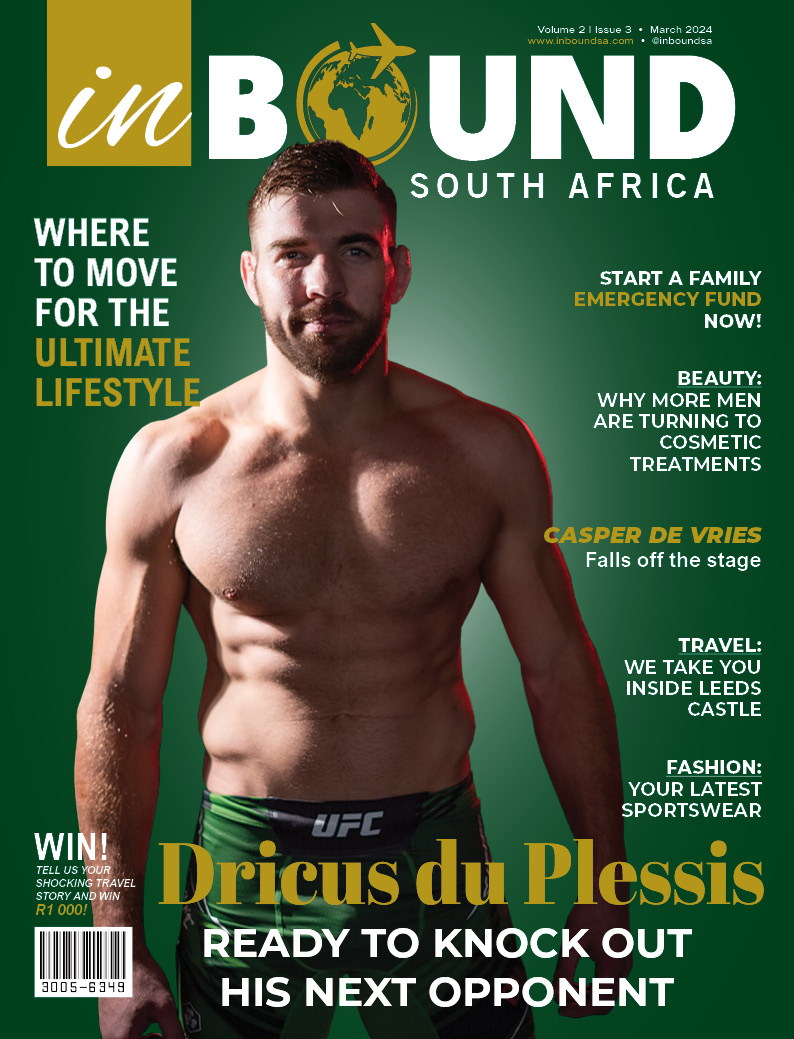
Media Xpose launches new travel magazine – InBound SA
South Africa (October 2023) – Media Xpose, one of the fastest-growing media groups in the country, has added yet another travel magazine to its already extensive media portfolio. InBound SA will cover arts and culture, adventure, events, celebrity news, shopping,...
Introducing “InBound SA” Magazine: A Blend of Business and Lifestyle Excellence
Media Xpose is proud to announce the launch of its latest endeavor, "InBound SA" magazine, an exciting publication that offers a unique blend of business insights and lifestyle content. (On distribution 1st November 2023) "InBound SA" is set to become the go-to source...
Media Xpose Spreads Joy on Mandela Day, Bringing Smiles to Children’s Faces
As the nation gathered to celebrate Mandela Day, Media Xpose, a media company, took the opportunity to bring joy to children's hearts. With a genuine spirit of generosity, the company donated toys and personalized gift bags to every child at the Brooklyn Chest...
Africa Day: Celebrating Unity, Diversity, and a Bright Future
On this special occasion of Africa Day, let us join hands and celebrate the rich tapestry of cultures, diversity, and unity that defines the African continent. As we commemorate the foundation of the Organisation of African Unity on May 25, 1963, let us reflect on the...
Media Xpose officially a Proudly SA member
Media Xpose joins Proudly SA as an official member, accentuating its commitment to high-quality standards, job creation and encourage buying local. Established in 2010, Media Xpose is a Level 2 BBBEE company with 60% black ownership, specialising in magazine...
Media Xpose nurturing young talent
As a responsible company that looks towards growth, building capacity and retaining talent is a key component of the business. Earlier this year, Ketsia Makola and Sherwin Kastoor were hired as Junior Salespersons, and have been afforded the opportunity to grow their...
Media Xpose acquires 50% stake in iXist
Media Xpose, a leading media house specialising in publishing, design, events and digital marketing, is proud to announce it has acquired a 50% stake in iXist – a website hosting company. “Digitisation continues to be a key factor for businesses, and as a...
Elroy van Heerden named Editor of the Year by SA Publication Forum
The entries were judged by a distinguished panel of judges and moderators whose evaluation criteria included: efficiently utilising resources to communicate with impact; project management; quality and taking initiative. “I am extremely humbled to receive this award....
What’s New Out There
The important evolution of HR
By Kim Naidoo, HR Manager, Anglophone Africa at Schneider Electric The role of Human Resources (HR) has certainly changed over the years. The advances in technology (AI) continues to evolve at a smashing pace reshaping and altering the way HR operates. Human Resources...
Beyond the test – ethical concerns spark debate on workplace drug testing
By Rhys Evans, Managing Director at ALCO-Safe The growing prevalence of workplace drug testing has ignited a fiery debate, shifting the spotlight beyond the act of testing itself to examine the integrity of results and the fairness of disciplinary repercussions. This...
Building a culture of productive meeting behaviour
by The Meetings Company founder Mark Kayser Drawing inspiration from thought leaders like Ray Dalio, founder of Bridgewater Associates, The Meetings Company integrates key insights into meeting behaviour to improve the way businesses approach collaboration. By...
Navigating digital fatigue: How Sensory Intelligence® can unlock success in the modern workplace
In the age of hybrid working, it's not all sunshine and rainbows. Daily digital fatigue is a significant consequence. The days of bustling commutes and lively offices have been combined with screen-bound isolation, with far-reaching consequences. Prolonged screen time...
Drug testing dilemma: urine detection vs. saliva testing – how to outsmart the ‘cheat’ to ensure reliable results
By Rhys Evans, Managing Director at ALCO-Safe Drug testing is a critical pillar of workplace safety and productivity. Among the various methods available, urine detection and saliva testing are two prevalent approaches, however, the central question that emerges in...
Workplace Bullying in the Digital Age – Old Problem, New Platforms
Almost every person who has ever worked with other people in a formal environment has faced so-called office politics. It’s part of the landscape and one well worth learning to navigate. However, once office politics cross over into workplace bullying, it becomes a...
How to identify CSI projects that create maximum social impact for a company
Corporate Social Investment is an integral part of modern business but choosing the right beneficiaries is crucial. Fundraising experts weigh in Corporate social investment has undergone considerable change since it was first introduced in the 1950s. Where before CSI...
Helping SA’s Hope Project 2024
Because their parents are in such financial straits, hundreds of children are showing up to school weary, undernourished, and in horrible clothing. Starving students snatching food from their peers while wearing threadbare clothing and worn-out shoes may sound like a...
From festive to focused: tips to overcome the post-holiday blues
Returning to the office after the holidays need not be an exercise in despair. While few of us will be unfamiliar with the feeling of having to get back into work mode after the holidays – a feeling the Urban Dictionary calls ‘after holiday syndrome’ – getting in the...
LEHLOHONOLO DAY CARE GETS BEAUTIFUL MAKEOVER
On 20 November 2023, in celebration of World Children's Day, and as part of the SUCCEED partnership between HOPE worldwide South Africa and Massmart, the team from the brand-new Builders Express store in River Square, Three Rivers, joined forces with the staff of...
Service Enquiry
Complete the form and we’ll be in touch with you.